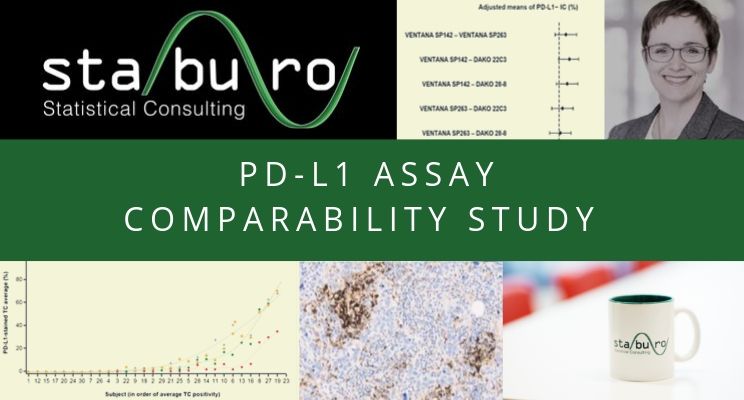
Staburo supported PD-L1 assay comparability study
PD-L1 assay comparability study published
Staburo supported the evaluation of the first multicentric analytical comparability study of PD-L1 expression in urothelial bladder cancer using four clinically developed immunohistochemistry assays. Statistical analyses included the investigation of inter-assay differences using ANOVA and intra-class correlations and the concordance for clinically relevant cut-offs based on Fleiss‘ kappa.
The results suggest that all four currently clinically relevant assays are analytically similar for the evaluation of PD-L1-stained immune cells and three (SP263, 22C3, and 28-8) for PD-L1-stained tumor cells.
The paper, which was recently published in Virchows Archiv, can be downloaded here (Staburo’s Statistics contribution is mentioned in the Acknowledgments): https://rd.springer.com/article/10.1007%2Fs00428-019-02610-z




Recent Comments